What is a Radical Resection of a Bone Sarcoma?
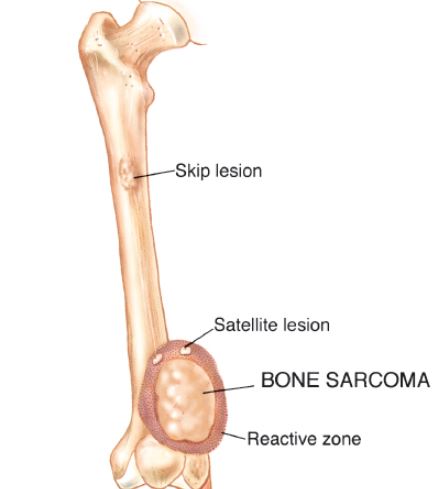
Since sarcomas spread microscopically a distance from the main tumor it is usually important to remove a cuff of surrounding normal tissue around the tumor. The more aggressive the tumor (usually more rapidly growing or called high grade) the wider the margin. Technically radical means removing the entire bone and muscle that contains the tumor. The extent of the bone sarcoma is determined on the preoperative MRI. Sarcomas should never be removed piece by piece as it will spread the tumor. Also, they should not be removed with an intralesional procedure that means entering the tumor and scraping it out of the bone. There are a few exceptions to this rule for some low grade and slow growing sarcomas that are less aggressive and have a much lower risk of coming back than the high grade or rapidly dividing bone sarcomas. Most high grade bone sarcomas are treated with chemotherapy before surgery (preoperative or neoadjuvant chemotherapy) and more chemotherapy after surgery (adjuvant chemotherapy). Radiation is rarely used in the treatment of bone sarcomas. Chemotherapy before surgery is aimed at killing the main tumor as well as any microscopic cells that have traveled in the body. It may also make saving the limb easier with the ability to save more normal tissues around the sarcoma. Sometimes there is major shrinkage of the sarcoma depending on the type of sarcoma. Sometimes a bone sarcoma may be determined to be unresectable meaning it needs an amputation. Preoperative chemotherapy may kill the sarcoma and make it resectable; capable of saving the limb instead of amputating it.